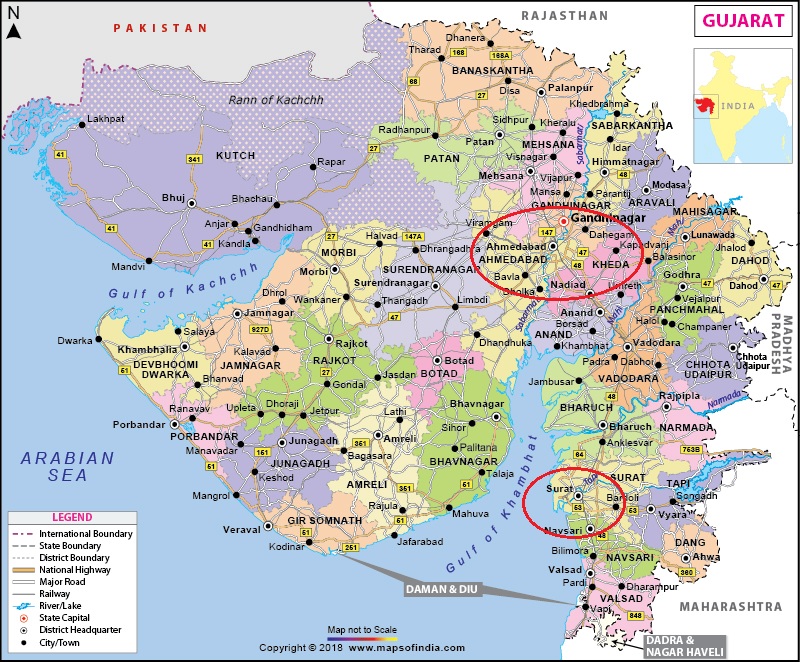
We examine MalariaWorld and other sources each week looking for interesting studies, especially those that look at the effect of poverty, nutrition, water quality and sanitation on the occurrence and severity of malaria. So we were drawn to ‘Socioeconomic and household water management determinants of malaria and other vector-borne disease prevention in Urban Gujarat, India’ by Batheja et al in this week’s MalariaWorld.
However the abstract reveals that nothing useful was found in the study, a socioeconomic and health survey in the cities of Ahmedabad and Surat, India, between September and November 2023. Data were collected from 4,074 households, comprising 15,484 individuals, and associations were examined between socioeconomic indicators, water availability, storage practices, and mosquito-borne disease incidence and prevention behaviours. Logistic regressions were used to identify significant predictors.
They found that self-reported disease prevalence was low, with 77 cases of malaria, dengue, and chikungunya, equivalent to 18.90 cases per 1,000 households. Socioeconomic factors such as wealth, caste, and family size were significantly associated with disease reporting and prevention practices. Households in the richest wealth quintile were more likely to adopt prevention measures, but less likely to perceive mosquito-related risks. Water management practices, particularly storage in clean large containers, were associated with increased disease symptoms and prevention measures, highlighting the complexity of vector control. Households with impermeable storage containers reported reduced use of active prevention measures.
They concluded that socioeconomic disparities and water management practices significantly influence malaria incidence and prevention behaviours. Targeted interventions prioritizing disadvantaged households, improved water storage practices, and enhanced investments in preventive care are essential to reduce vector-borne disease vulnerability and accelerate India’s malaria elimination goals.
What a huge nothing burger! Malaria was reported for just 0.40% of study participants. This is very low compared to incidence of 61% in Bas-Uele province of DRC reported last week. Obviously, with such a low incidence it is impossible to draw any statistically significant conclusions from the data. The results reported relate more so to behaviours to prevent these supposedly mosquito transmitted ailments.
If this is the most relevant study the researchers could conduct, can we deduce that in common with much of the rest of Asia, malaria is ceasing to be a major health problem in India?